DETAILED ESCHERICHIA COLI FACT SHEET
Although is may be hard to believe, some types of E. coli are actually good and help out your body! Right now, at this very moment, there are E. coli bacteria lining your intestine and they’re helping you digest your food and stopping other bad bacteria that may have snuck in with your meal from making you sick. Without those good E. coli being there, who knows what would happen?
However, as we hear on the news and in the paper, not all E. coli types are our friends. One type in particular, E. coli O157:H7, is a bad bacterium, which can make us very sick if it gets inside of our bodies. Read on to find out what these bacteria are all about. For general information about bacteria, please see the “Bacteria” fact sheet.
What is Escherichia coli?
Escherichia coli, also referred to as E. coli, is a type of fecal coliform (see definition below) bacteria that is found in the intestines of healthy warm-blooded animals and humans. Most E. coli strains are harmless and serve a useful function in the body by stopping the growth of harmful bacteria species and by making necessary vitamins. However, some strains can be opportunistic pathogens, while others can cause gastrointestinal illness in healthy humans when ingested. An opportunistic pathogen is an organism that normally lives inside a host without causing injury, but can cause infection in people with weakened immune systems. E. coli is present in the large intestine, so it will be present in fecal matter from humans and animals. If recent contamination of water sources with sewage or animal waste has occurred, E. coli will be present.
E. coli was identified in 1885 by Theodor Esherich, and is a member of the family Enterobacteriaceae – a large family of bacteria that live in the intestine. Soon after it was discovered, it became a popular lab organism because it could be grown quickly on different media. E. coli can grow either in the presence or absence of oxygen and is able to use different sources for its food requirements.
Source: http://www.about-ecoli.com/
What is a Fecal Coliform?
A fecal coliform is a bacterium that is associated with animal or human waste and usually lives in human or animal intestinal tracts. A common example of a fecal coliform is E. coli, as mentioned above. The presence of fecal coliforms in water is a strong indication of recent sewage or animal waste contamination.
What is E. coli O157:H7?
Unlike the bacteria E. coli that was identified in 1885, E. coli O157:H7 was not identified until 1975 at the U.S. Centers for Disease Control. It wasn’t until another seven years after, in 1982, that this strain of E. coli was determined to be a cause of enteric disease when the bacteria was linked to several cases of bloody diarrhea. This association resulted in the O157:H7 strain to be designated as an enterohemorrhagic E. coli. It was given this name because of its association with damage to the epithelium of the intestine.
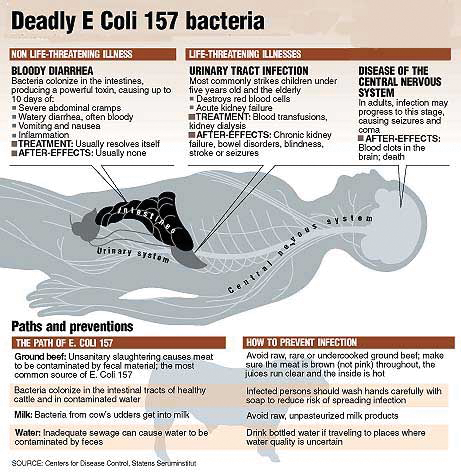
Because there are so many different strains of E. coli, it must be classified into different groups. These groups are called serogroups, and each consists of one or more different subgroups, or serotypes. Serotypes are groups of bacteria that are very similar to each other, but that can still be told apart by certain characteristics found on the surface of the bacterial cell. The combination of letters and numbers in the name E. coli O157:H7 refers to the specific markers found on the surface of the bacterium and is what distinguishes it from other types of E. coli. The E. coli serotype O157:H7 is a rare variety of E. coli that produces large quantities of powerful toxins (poisons) that cause severe damage to the lining of the intestine, and that can also cause severe illness. Hemorrhagic colitis is the name of the acute (short but with a severe course) disease caused by E. coli O157:H7.
What Are the Symptoms and the Incubation Time?
After someone ingests a sufficient quantity of E. coli O157: H7, the bacteria travel through the stomach and small intestine, attach themselves to the inside surface of the large intestine and causes inflammation of the intestinal wall. The infective dose is thought to be as low as 10 infectious particles.
The symptoms associated with E. coli O157:H7 vary with each infective case. Severe abdominal cramping and diarrhea that is initially watery, but becomes grossly bloody as the infection period continues characterize illness caused by E. coli O157:H7. Vomiting occurs occasionally, and little or no fever is present. Some infections will not cause bloody diarrhea (watery diarrhea only), or won’t show any symptoms at all. The incubation period (period from ingestion of the bacteria to the start of the symptoms) for this disease is usually three to nine days. Both shorter and longer periods have been recorded, but symptoms do not usually appear in a time period of less than 24 hours.
In addition to the above symptoms, infection with E. coli O157:H7 can cause a complication called Hemolytic Uremic Syndrome (HUS) in some people - especially in children under five years of age and the elderly. See the explanation of HUS in the ‘Am I at severe risk for disease?’ section below.
How Long do the Symptoms Last?
In most infected individuals, recovery from the symptoms of E. coli O157:H7 occurs in five to ten days, with the average being about one week. The illness usually resolves without the use of antibiotics or other treatments and clears up without any long-term problems. It is thought that the use of some medicines, such as anti-diarrheal agents, may even increase the chances of developing complications and their use should therefore be avoided.
How is it Diagnosed?
Hemorrhagic colitis (infection with E. coli O157:H7) is diagnosed by detecting the bacterium in the feces of an infected individual. Most laboratories that culture feces samples do not test for E. coli O157:H7, so if infection is suspected, it is important to request that the sample be tested accordingly. Anyone who develops severe bloody diarrhea should get his or her feces tested for E. coli O157:H7. Confirmation of the outbreak cause can be obtained by detecting the same strain of E. coli from both the fecal sample and the suspected source alike.
Who is at Risk?
While everyone is susceptible to becoming infected with E. coli O157:H7, children under the age of five, the elderly and the immunocompromised (those with weakened immune systems such as cancer and AIDS patients) are at a greater risk of severe illness and also have an increased chance of developing long term complications from the infection. In 2015, there were 634 reported cases of E. Coli infections across Canada in people of all ages.
Am I at Severe Risk for Disease?
As mentioned in the previous section, all people are susceptible to E. coli infection but children younger than five years of age, the elderly, as well as those who are immunocompromised, are at an increased risk of developing complications from infection with E. coli O157:H7 – namely, Hemolytic Uremic Syndrome (HUS). About 2%-7% of infections will lead to this complication that is characterized by haemolytic anaemia (too few red blood cells in bloodstream resulting in insufficient oxygen delivery to tissues and organs) caused by the destruction of red blood cells) and renal failure (permanent loss of kidney function). In the United States, HUS is the principal cause of acute kidney failure in children, and most cases of HUS are caused by E. coli infection. HUS is a life-threatening condition usually treated in an intensive care unit, with blood transfusions and kidney dialysis often being required. Even with intensive care, the death rate for HUS is 3%-5%.
In addition to HUS, the elderly are also at increased risk of developing a more severe complication called Thrombotic Thrombocytopenic Purpura (TTP). The symptoms are similar to those of HUS, but TTP also induces fever and neurological symptoms. In the elderly, this illness can have a mortality rate as high as 50%.
Hemolytic Uremic Syndrome
Hemolytic Uremic Syndrome, also referred to as HUS, was first described in 1955 and is now recognized as the leading cause of kidney failure in children. HUS is a severe life threatening complication that will develop in 5%-10% of individuals infected with E. coli O157:H7. In fact, E. coli O157:H7 is responsible for over 90% of the cases of HUS that develop in North America and many researchers now believe that it is the only cause of HUS in children.
HUS will suddenly appear five to nine days after the onset of the symptoms associated with E. coli O157:H7, but can occur as early as one to two days after diarrhea begins. HUS develops when the bacteria can enter the bloodstream through the inflamed intestine wall and release a specific chemical system known as Shiga-like toxin (SLT). This toxin will attach to receptors on the inside surface of the endothelial cells (blood vessel cells) and subsequently cause damage.
Once the E. coli infection has developed into HUS, there is no known medication to stop its progression. HUS is characterized by rapid development of haemolytic anaemia and thrombocytopenia (a decrease in the number of platelets in the blood resulting in a decreased ability for blood clotting) in conjunction with variable degrees of CNS (central nervous system) dysfunction (i.e. seizures, coma, etc...). The active stage of the disease is usually one to two weeks and it is during this time period that many different complications are possible. About 50% of patients will require kidney dialysis, 25% will develop pancreatitis (inflammation of the pancreas), 25% will experience seizures and 5% will suffer from diabetes mellitus. The majority of these patients will require blood transfusions and will develop complications common to the critically ill. HUS is a frightening illness that even in the best of medical facilities has a mortality rate of 5%.
The survivors of HUS will develop different problems. Approximately 5% will eventually develop end stage kidney disease with dialysis or transplant being required, and another 5%-10% will experience neurological or pancreatic problems that will impair quality of life. Even children who seem to have recovered from HUS will develop hypertension (persistently high arterial blood pressure), urinary abnormalities and/or renal (kidney) insufficiencies during long-term follow-ups.
In Canada, HUS is relatively common with about 75-90 cases being identified in children each year. The risk of HUS in children brought to medical attention for an E. coli O157:H7 infection is approximately 8%-10%. Nonetheless, 20%-25% of children won’t have any visible evidence of bloody stools in two weeks before presenting with HUS.
Thrombotic Thrombocytopenic Purpura
Generally recognized as “adult HUS,” thrombotic thrombocytopenic purpura (TTP) is a clinical syndrome defined by the presence of thrombocytopenia (decreased platelets in the blood) and microangiopathic haemolytic anaemia (fragments of red blood cells circulating in bloodstream). This syndrome is brought upon by many causes, one of which is infection with E. coli O157:H7. All possible causes act by inducing endothelial cell damage. An endothelial cell is a small thin cell, a layer of which lines the inside of body cavity and blood vessel surfaces. This damage causes a chain of events to occur that will ultimately result in multi-organ abnormalities.
The symptoms of TTP vary. Vomiting and diarrhea are present and many patients complain of malaise (body discomfort) and weakness. Hypertension (persistently high arterial blood pressure) is also often present. Neurological signs may be present after a few days if illness and some of these include: headache, cranial nerve palsies (paralysis of the cranial nerves), hemiparesis (paralysis affecting only one side of the body), dysphasia (impairment of speech and verbal comprehension)/aphasia (partial or total loss of the ability to articulate ideas or comprehend spoken or written language), confusion, stupor (state of reduced or suspended sensibility), coma and seizures. Bleeding associated with the gastrointestinal tract is also common.
The treatment for TTP is aimed at the changes that have occurred in the body. Some patients will fully recover while in others, the disease assumes a prolonged course, characterized by recurrent attacks of TTP. The treatment involves plasmapheresis (daily plasma volume exchange), which is continued until the platelet count normalizes. This may take up to 10 days or longer to obtain complete remission (the subsiding of symptoms) in seriously ill patients. Plasma exchange does not cure TTP, but rather controls the disease until spontaneous remission occurs.
How Does E. coli O157:H7 Spread?
E. coli O157:H7 can live in the intestines of healthy cattle and will not make the animals that have it sick – they are merely a reservoir (a ‘holding tank’) for the bacteria. Meat can become contaminated during slaughter, and organisms can be mixed into beef when it is ground. Eating meat, especially ground beef that has not been sufficiently cooked to kill E. coli O157:H7 can cause infection. Contaminated meat will both look and smell normal, so it is impossible to distinguish between safe and infected meat. It also possible that bacteria present on the cow’s udders or on the milk equipment may get into raw milk, with the risk of infecting those who consume it if the milk is not pasteurized beforehand. Raw milk was the source of an E. coli O157:H7 school outbreak in Canada. Other sources of infection include: consumption of sprouts, lettuce, cheese curds, salami, unpasteurized juice and swimming in or drinking in sewage-contaminated water.
E. coli O157:H7 can also live in the intestines of humans and is spread to others via the fecal-oral mode of transmission. The bacteria in the feces of those who are infected can be passed from person to person if poor hygiene habits (such as inadequately washing your hands) are practiced. This type of spreading is especially common in toddlers who are not yet toilet trained – family members and friends of these children are at a high risk of becoming infected. Young children continue to shed the bacteria in their feces up to two weeks after their illness resolves.
How Can I Prevent Getting E. coli O157:H7?
The Centers for Disease Control and Prevention (CDC) suggests many actions that may be taken to prevent E. coli infection. To avoid getting infected, you should consider following this list:
Avoid swallowing lake or pool water while swimming, especially pool water in public swimming facilities.
Avoid unpasteurized milk.
Make sure that persons with diarrhea, especially children, wash their hands carefully with soap after going to the bathroom to reduce the risk of spreading infection, and that persons wash hands after changing soiled diapers. Anyone with a diarrheal illness should avoid swimming in public pools or lakes, sharing baths with others, and preparing food for others.
Cook all ground beef and hamburger thoroughly. Because ground beef can turn brown before disease-causing bacteria are killed, use a digital instant-read meat thermometer to ensure thorough cooking. Ground beef should be cooked until a thermometer inserted into several parts of the patty, including the thickest part, reads at least 160 degrees Fahrenheit. Persons who cook ground beef without using a thermometer can decrease their risk of illness by not eating ground beef patties that are still pink in the middle.
If you are served an undercooked hamburger or other ground beef product in a restaurant, send it back for further cooking. You may want to ask for a new bun and a clean plate, too.
Avoid spreading harmful bacteria in your kitchen. Keep raw meat separate from ready-to-eat foods. Wash hands, counters, and utensils with hot soapy water after they touch raw meat. Never place cooked hamburgers or ground beef on the unwashed plate that held raw patties. Wash meat thermometers in between tests of patties that require further cooking.
Drink only pasteurized milk, juice, or cider. Commercial juice with an extended shelf-life that is sold at room temperature (e.g. juice in cardboard boxes, vacuum sealed juice in glass containers) has been pasteurized, although this is generally not indicated on the label. Juice concentrates are also heated sufficiently to kill pathogens.
Wash fruits and vegetables thoroughly, especially those that will not be cooked. Children under five years of age, immunocompromised persons, and the elderly should avoid eating alfalfa sprouts until their safety can be assured. Methods to decontaminate alfalfa seeds and sprouts are being investigated.
Drink municipal water that has been treated with chlorine or other effective disinfectants.
How do I Prevent Spreading it to Others?
The guidelines given above for how to prevent getting E. coli O157:H7 can also be applied as the suggestions for how to prevent spreading it to others if you do indeed become infected. The main guidelines that should be followed with extra care are listed below:
Wash your hands thoroughly after using the bathroom and before preparing food for others. Food preparation should really be avoided all together while suffering from diarrheal illness.
Avoid swimming in lakes or pools while you have diarrhea. This could contaminate the water and infect other swimmers.
Make sure that persons with diarrhea, especially children, wash their hands carefully with soap after bowel movements to reduce the risk of spreading infection, and that persons wash hands after changing soiled diapers.
What is the Treatment for O157:H7?
As discussed above in previous sections, most people who become infected with E. coli O157:H7 recover without antibiotics or other specific treatments in five to ten days. Some medical researchers believe that taking anti-diarrheal medications such as Imodium may even increase the risk of complications. Therefore, apart from good supportive care and home therapy treatments, such as staying hydrated and paying close attention to nutrition, there is no specific treatment for E. coli O157:H7.
How Prevalent is E. coli O157:H7 in Surface Water/Well Water?
E. coli O157:H7 is an emerging cause of foodborne and waterborne illness; a strain that can produce a powerful toxin that will cause severe illness. Although most infections are believed to have come from eating undercooked ground beef, many outbreaks have been linked to water. In 1999, people became sick after drinking contaminated water in New York and swimming in contaminated water in Washington. In May 2000, a water-borne outbreak caused by E. coli O157:H7 was detected in the rural town of Walkerton, Ontario, Canada. By the time the outbreak was brought under control in mid-June more than 2,300 cases and seven deaths had been reported. It was not until 1993 that this organism became reportable for all of Canada. Below is a table indicating the reported cases of E. coli O157:H7 for a nine year inclusive period from 1990-1998. Both total number of cases and cases per 1,000 are reported.
There have also been numerous other outbreaks with water identified as the source of infection.
E. coli O157:H7 comes from animal and human wastes, and during heavy rainfalls, snow melts, and other precipitation, it may be washed into creeks, rivers, streams, ponds or groundwater. When these waters are used as sources of drinking water and the water is not properly treated, E. coli may end up in the drinking water with the potential of infecting large numbers of people.
How Can We Protect Our Water Supplies?
About 89% of Americans receive water from community water systems that meet all health based standards. If extra precaution is desired, it is advised to bring water to a rolling boil for one minute, and for a longer time period if at higher altitudes. If you get your water from a private well, your well should be tested for the presence of E. coli. If the tests are positive, there are three steps that should be followed:
1. Begin boiling all water intended for consumption
2. Disinfect the well according to health department procedures
3. Consistently monitor water quality to make certain that the problem does not reoccur
If contamination is a recurring problem, drilling a new well or installing a point-of-entry disinfection unit (using chlorine, ultra-violet light or ozone) are all recommended modes of action.
Is My Water Safe? How Can I Tell?
If you get your water from a public water system, your water system is required by law to notify you if your water is not safe. If you have a private well, it should be tested periodically to ensure it is free from contamination. It is usually not necessary to test specifically for E. coli O157:H7 because if this strain is present in your well, it is highly likely that other strains will also be present. If any strain of E. coli is detected, the water should not be consumed unless it is thoroughly treated first.
The Prairie Provinces in Canada have a unique water situation in that a large proportion of the rural population relies on water from dugouts and shallow aquifers that drain or are recharged from agricultural fields with high numbers of livestock. The water present in these sources is hard to disinfect because part of the disinfectant used is consumed by the excess amount of organic material present in the water source from the agricultural run-off and these reactions cause by-products that can be carcinogenic. Other forms of water supplies include an extensive network of low-pressure water pipelines distributing water that may have received some form of treatment, but is supplied without regular monitoring or maintenance to rural users. The poor water quality in rural prairie areas may be linked to high levels of waterborne illness, such as E. coli O157:H7. Poor quality rural water sources, combined with ineffective water treatment, results in the consumption of unsafe drinking water by many rural citizens, which puts them at an increased risk of becoming infected with a waterborne pathogen such as E. coli O157:H7.
What Are Some Ways I Can Treat My Water to Ensure its Safety?
Water, especially water from a private water source like a well, can be treated using chlorine, ultra-violet light, or ozone, all of which act to kill or inactivate E. coli. Systems using surface water sources are required to disinfect to ensure that all bacterial contamination, such as E. coli, is inactivated. Systems using ground water sources are not required to disinfect in all jurisdictions, but the introduction in the United States of the Ground Water Rule dispelled most myths that groundwater is safe to drink without treatment. Indeed during the past decade the majority of waterborne illnesses in the U.S. originated from groundwater.
How Does the U.S. Environmental Protection Agency Regulate E. coli?
The following in an excerpt taken from the USEPA website.
“According to EPA regulations, a system that operates at least 60 days per year, and serves 25 people or more or has 15 or more service connections, is regulated as a public water system under the Safe Drinking Water Act. If a system is not a public water system as defined by EPA’s regulations, it is not regulated under the Safe Drinking Water Act, although, it may be regulated by state or local authorities.
“Under the Safe Drinking Water Act, EPA requires public water systems to monitor for coliform bacteria. Systems analyze first for total coliform, because this test is faster to produce results. Any time that a sample is positive for total coliform, the same sample must be analyzed for either fecal coliform or E. coli. Both are indicators of contamination with animal waste or human sewage.
“The largest public water systems (serving millions of people) must take at least 480 samples per month. Smaller systems must take at least five samples a month unless the state has conducted a sanitary survey – a survey in which a state inspector examines system components and ensures they will protect public health – at the system within the last five years.
“Systems serving 25 to 1,000 people typically take one sample per month. Some states reduce this frequency to quarterly for ground water systems if a recent sanitary survey shows that the system is free of sanitary defects. Some types of systems can qualify for annual monitoring.
“Systems using surface water, rather than ground water, are required to take extra steps to protect against bacterial contamination because surface water sources are more vulnerable to such contamination. At a minimum, all systems using surface waters must disinfect. Disinfection will kill E. coli O157:H7.”
Ninety-six percent of all violations of the Total Coliform Rule in the U.S. are committed by communities less than 10,000 people so the logic, other than economic, of less sampling for smaller communities is simply not there.
Will a Water Filter Work to Keep E. coli Out of My Water?
Most in-home water filter will not prevent E. coli O157:H7 from getting into your tap water. If you are concerned about the safety of your tap water, it is recommended to boil your water before using it to cook or to drink.
Did you know that our Operation Water Health program is available free of charge to teachers worldwide and provides the teachers with all of the lesson plans and information they need to teach students about what safe drinking water is, what unsafe drinking water is, and what health problems can be caused by unsafe drinking water? Please help us to keep our Operation Water Health program up-to-date! Please chip in $5 or donate $20 or more and receive an Official Donation Receipt for Income Tax Purposes.